About Kidney Exchange
The Challenge
Disease Background
Chronic kidney disease (CKD) is a long-term condition where people experience a loss of kidney function.
CKD mostly develops slowly, without initial symptoms. It becomes progressively more debilitating at later stages.
When a person’s kidneys fail (end-stage kidney disease), they need life-long dialysis unless they can obtain a kidney transplant.
People with CKD suffer from numerous serious symptoms and limitations, such as frequent hospitalisation, depression, pain and fatigue.
When someone is on dialysis, this takes up at least 12 hours a week of their time.
Dialysis cost the UK National Health Service an estimated £34,000 per year per patient in 2023.
CKD can be fatal: by 2019, CKD accounted for 2.36% of total deaths in the European Union, with an expected annual increase of 2.38%.
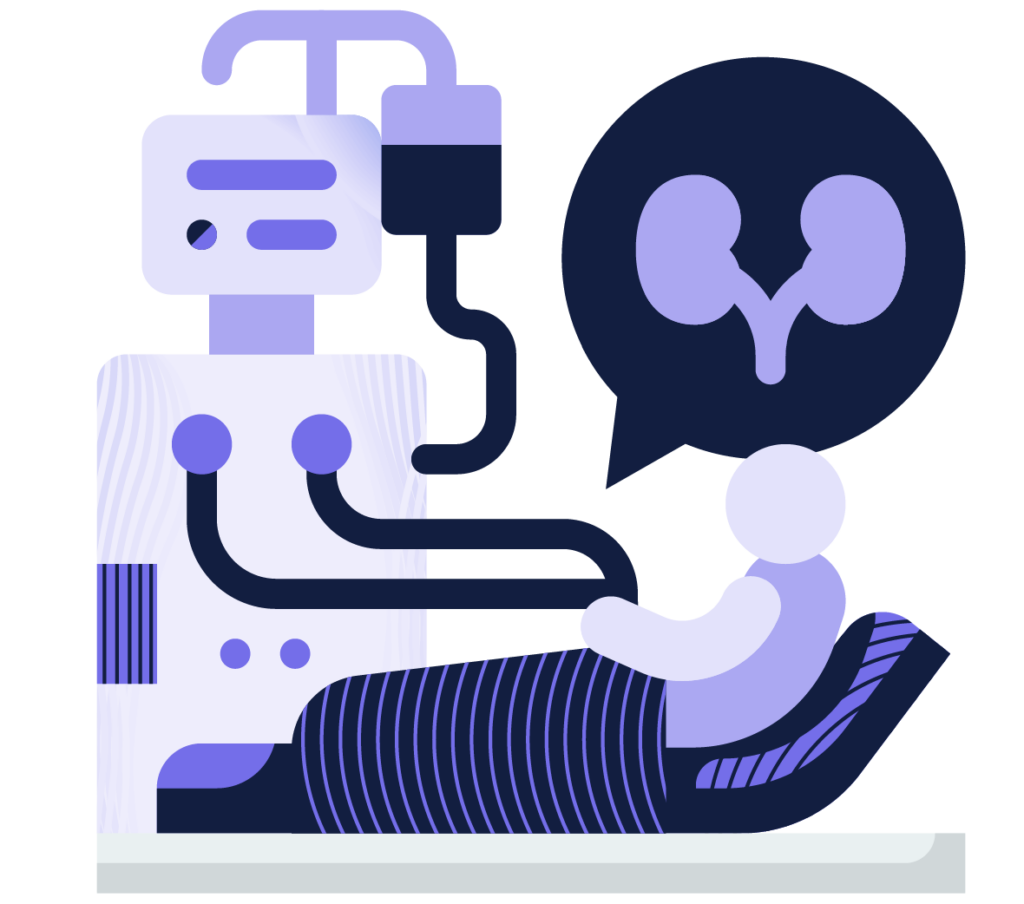
Figure 1: A patient on dialysis
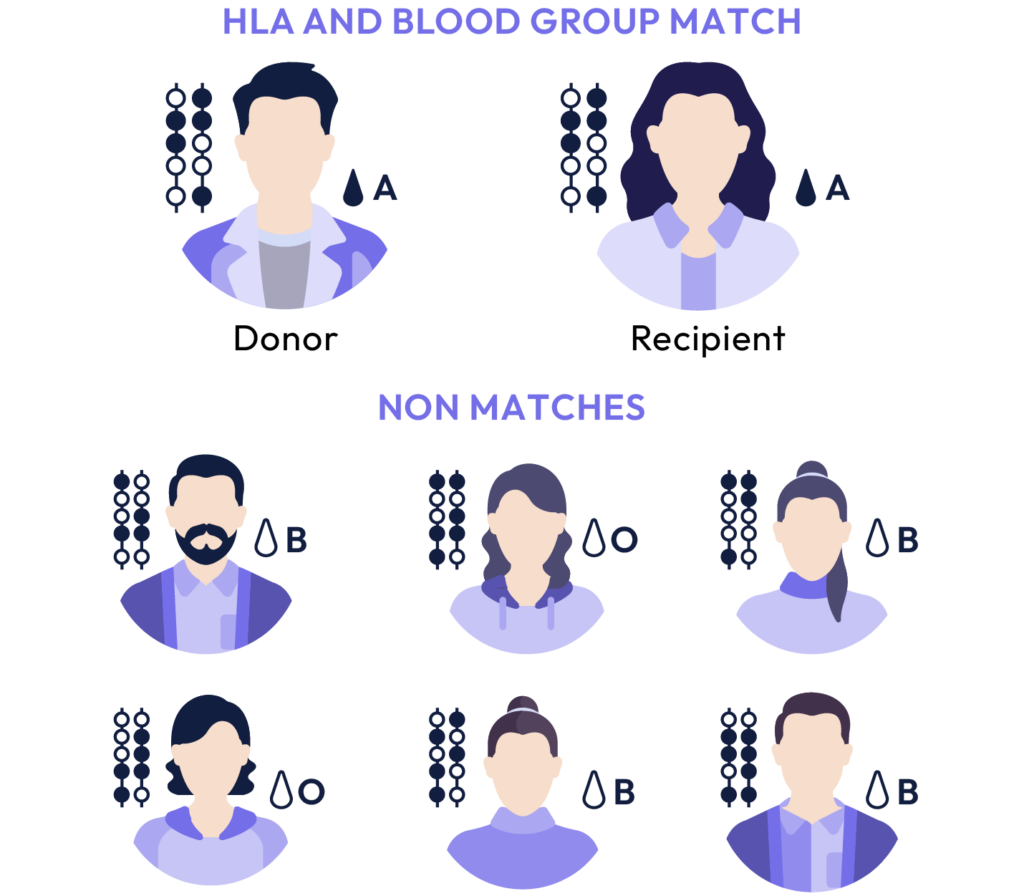
Figure 2: Example of an HLA and blood group match
Approximately 40% of kidney donors and recipients are currently not a match.
Unmet Needs of CKD
A kidney transplant from a living donor results in optimal survival rates, compared with a deceased donor.
Living donors may choose to donate to someone they know (‘directed’ donation) or to someone they do not know (‘non-directed’ or ‘altruistic’ donation).
However, in the UK alone between April 2022 and April 2023:
5,600 people were waiting for a kidney transplant.
270 people died while being on the waitlist.
Not all donors are compatible:
Compatibility is based on the donor and recipient's blood groups (ABO-compatibility), and also the absence of donor-specific human leukocyte antigens that are unacceptable to the recipient (HLA-compatibility); see Figure 2.
If the donor and recipient are not compatible, this may lead to serious consequences such as transplant rejection or graft-versus-host disease.
Solution:
Kidney Exchange
A Kidney Exchange Programme (KEP) reallocates donors to more appropriate recipients, based on blood type and HLA compatibility when:
A CKD patient has a donor willing to donate a kidney who is not a good match
Case 1
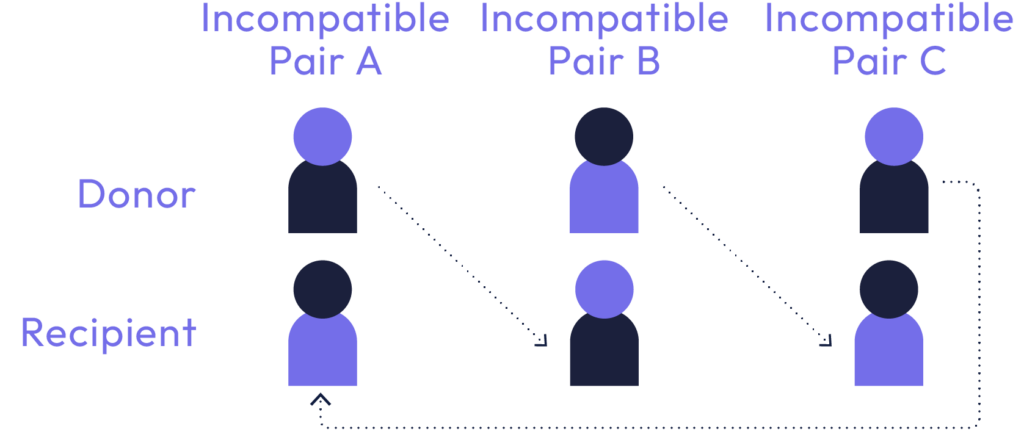
This is an example of a kidney exchange, in the form of a “cycle”, involving three donor-recipient pairs. Donor A is the willing but incompatible donor for recipient A, and similarly for pairs B and C. Here, donor A gives a kidney to recipient B, donor B gives a kidney to recipient C, and donor C gives a kidney to recipient A.
A kidney from a non-directed (altruistic) donor becomes available
Case 2
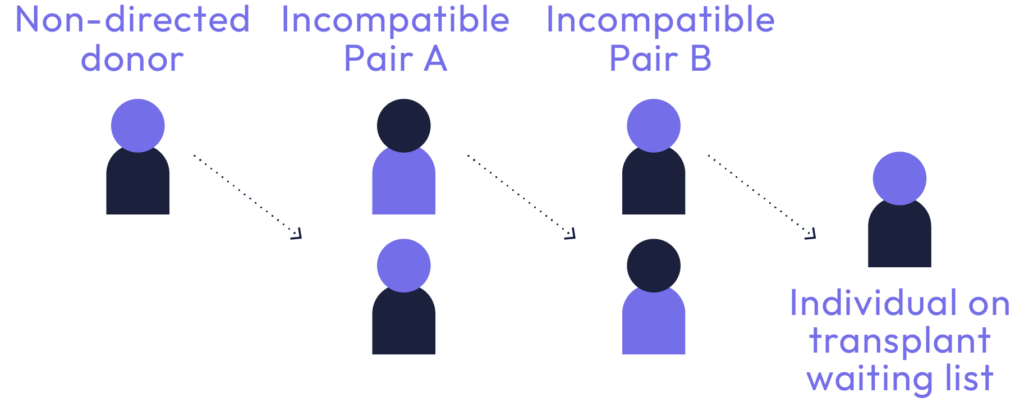
This is an example of a kidney exchange, in the form of a “chain”, triggered by a non-directed donor (someone who wishes to give a kidney but does not have an identified recipient) and involving two further donor-recipient pairs. Here, the non-directed donor gives a kidney to recipient A, donor A gives a kidney to recipient B, and donor B gives a kidney to a recipient on the deceased donor waiting list.
Kidney Exchange Programmes offer an important solution to the challenge of incompatible donors and recipients, increasing the chances of people receiving the kidney transplant that they need.
Unmet Needs of Kidney Exchange Programmes
Often, KEPs exist only at the hospital or national level, enrolling only a limited number of donor and recipient pairs.
Few European countries operate large national or international KEPs.

These factors may result in a reduced chance of finding possible donor and recipient matches.